I saw a fascinating case last month. The patient was a high level 13 year old baseball player who developed pain in the region of his knee cap (technically called the patella).
He did not have any traumatic injury, so I had a low suspicion of an injury like a patellar fracture, nor did I suspect a traumatic injury his ACL ligament or meniscus.
He was just starting his growth spurt. Youth athletes are vulnerable to a different class of injuries than adult athletes. The patellar ligament is what I call a structural complex, connecting the lower portion of the knee cap (the inferior pole of the patella) to a small bump on the shin called the tibial tuberosity.
This patellar ligament complex can be injured in different locations, depending on age:
- Age 11-12- at the inferior pole of the patella, an injury called Sinding-Larsen-Johannson syndrome
- Age 13-14- at the tibial tuberosity (where the patellar ligament attaches to the tibia)- called Osgood Schlatter syndrome.
The age ranges for SLJ and OS are approximate, but as a general rule SLJ occurs earlier in adolescence, and the more common OS occurs a few years later. Their timing is based on when the bony processes, called an apophysis, fuses to the rest of the bone.
By late adolescence, the apophyses have fully fused, so we don't see these injuries much by an athlete's late 20s. We may still see irregularities in the bone, but these are remnants of a prior injury, and rarely the cause of injury itself. Instead, in athletes who are past puberty, the most common site of injury is within the patellar ligament itself (usually closer to the patella than the tibial tuberosity), a a condition called patellar tendinopathy, or jumper's knee.
In our clinic at Lake Washington Sports & Spine, Dr. Hyman and I like to use high-resolution musculoskeletal ultrasound to image the patellar ligament complex. Ultrasound is a particularly great imaging tool for assessing tendons, for the following reasons:
1. It has the highest spatial resolution- 5-10 times higher than MRI
2. Real time assessment- it is the only imaging test that adds in actually touching the patient, so we can confirm that the area being imaged is actually painful. This is particularly valuable in rough-and-tumble athletes with a history of prior injuries, to help clarify whether the injury is new
3. Fantastic tissue differential- ultrasound is great at distinguishing between different tissue types
To give an example of an ultrasound image of a patellar-ligament complex injury, the image below is that of Sinding Larsen Johannson syndrome in an 11 year-old elite-level soccer player. The yellow box shows irregularity in the apophysis of the inferior pole of the patella (to help with orientation, left is superior, right is inferior)
Getting back to the 13 year old baseball player, based on his age and pain near the patella, I was anticipating that he may have SLJ syndrome. However, his pain was located higher (on the superolateral portion of his knee cap).
Indeed, as the image below shows, the patella looked pristine in the center, with a smooth cortex
However, when I moved the probe laterally, I could see two disruptions in his cortex
This is a case of what is called a bipartite patella. The superolateral portion of the patella never fused to the remaining part of the patella. The x-ray image below shows the non-union of the bipartite patella, along with the planes of the two images above
How did I use this information clinically:
1. Relative non-use
2. Physical therapy. Particular focus include stretching of the rectus femoris at the hip, since we wanted to limit traction of the quad distally
3. Avoiding NSAIDs. The specific mechanism can interfere with healthy collagen synthesis, essential in this growing athlete
4. Regular icing
This athlete did great, and was able to return to sport in 1 month
Tuesday, May 26, 2015
Wednesday, May 6, 2015
Exercise Is Medicine! Dr. Hyman Trains with the US Medical Soccer Team in Atlanta (www.usmedicalsoccerteam.org)
May 2015
I just returned from a wonderful weekend devoted to community service, physician-kinship and arduous physical training in Atlanta, Georgia.
I met up with approximately 30 other physician colleagues from around the USA to prepare for our upcoming hosting of the World Medical Football Congress (WMFC), set to take place in Long Beach, CA, at the end of June 2015. We are the US physicians who make up the US Medical Soccer Team (USMST). (www.usmedicalsoccerteam.org)
We had 4 separate training sessions over the weekend and now I am enjoying a day of muscle recovery (but brain exercise) at work. Our coach performed well to get us organized into a formation that should allow us to win games and make it to the knock out round of the tournament.
We arrived Friday afternoon, and met at the GW Carver Boys & Girls Club of Metro Atlanta, and we delivered our own “Healthy, Fit and Smart” education program to approximately 100 disadvantaged children. The kids were wonderful — engaging, energetic, and with every small success answering our questions, their eyes beamed, and the potential for these children to absorb knowledge like sponges was palpable. Highlights included one child answering ‘potassium’ as one of the 5 food groups (e.g. fruits, vegetables, grains, meats/fish, dairy), and another answering “eight hours a day” for the minimum time doctors recommend children watch TV (to be clear, there are no minimum daily requirements for TV watching!). I think all of us doctors left the event grateful to the children from whom we continue to learn each time we deliver the Healthy, Fit and Smart program.
Our USMST potential is strong. We will compete against physician national soccer teams from 18 different countries. We’ve not made it past the early stages in prior tournaments. In truth, we are a perennial underdog. This year the team has several new physician-athletes, and we have high hopes to make our way to the knock out round of the tournament.
The physicians with whom I play are from all fields, and many are naturalized US citizens. We have a trauma surgeon originally from Caracas, Venezuela, a vascular surgeon from Lima, Peru, an Internist from Romania, and a Family Physician from Trinidad and Tobago. A good number of our physicians are originally from Iran. We are a real melting pot. Our dinner conversation usually surrounds soccer, but of course we banter quite a bit about medical topics as well.
So as our June training in Seattle and our summer tournament draw near, I reflect on how grateful I am that I can continue to push my fitness to new levels and compete on a ‘mini-world stage.’ I thank my family and my work team at LWSS without who's support I could not make this happen.
Monday, May 4, 2015
The danger of the "cost containment" industry
There is a recent article in the New Yorker that highlights the dangers of health care over-utilization. It is a thoughtful, well-written article.
However, I suspect the governmental reaction to this article will be very anti-patient. As an example, one of the major insurance companies we work with just published a bulletin requiring many musculoskeletal injections to undergo prior authorization by an outside company, CareCore National. Their "Musculoskeletal Pain Management Criteria" document is 134 pages of guidelines that will limit what physicians are able to perform in office.
The current "big medicine" solution to over-utilization is to create an extra-layer in the health care process, and that extra layer has a large cost. As a consequence, of the total money the US spends on health care, a higher % will go to administration, and a lower % will go to the actual delivery of care.
One of the terms that is thrown around a lot in medicine is "third party." What patients need to recognize is that when there are increasing bureaucratic layers added in healthcare, the PATIENT becomes the third party. We have many patients who have left big-system medicine practices and are now seen by us, because they are sick of being treated like a widget. This happens because the physician is so busy focusing on compliance requirements from the insurance company and/or the health system where the physician is employed.
Are there people who abuse the system? Of course! But government intervention actually leads to MORE abuse. For the small clinical practice who plays by the rules, these additional regulations just add additional cost and compliance burden, which gets in the way of good care. There is only one class of doctors who afford the time and resources to hiring extra staff to handle specious treatments, and those are the serial abusers of the system. The New Yorker itself did a fine expose piece in 2009 about these serial abusers in McAllen, Texas, who took advantage of low income, non-English speakers to run up costs. This type of abuse would not be possible except that there are large central systems to manipulate, and because they were such abusers, it was worthwhile to devote resources to this manipulation.
We at Lake Washington Sports & Spine will continue to fight against this trend. We will aim to be judicious in use of resources, but we will always prioritize the needs of the patient first.
However, I suspect the governmental reaction to this article will be very anti-patient. As an example, one of the major insurance companies we work with just published a bulletin requiring many musculoskeletal injections to undergo prior authorization by an outside company, CareCore National. Their "Musculoskeletal Pain Management Criteria" document is 134 pages of guidelines that will limit what physicians are able to perform in office.
The current "big medicine" solution to over-utilization is to create an extra-layer in the health care process, and that extra layer has a large cost. As a consequence, of the total money the US spends on health care, a higher % will go to administration, and a lower % will go to the actual delivery of care.
One of the terms that is thrown around a lot in medicine is "third party." What patients need to recognize is that when there are increasing bureaucratic layers added in healthcare, the PATIENT becomes the third party. We have many patients who have left big-system medicine practices and are now seen by us, because they are sick of being treated like a widget. This happens because the physician is so busy focusing on compliance requirements from the insurance company and/or the health system where the physician is employed.
Are there people who abuse the system? Of course! But government intervention actually leads to MORE abuse. For the small clinical practice who plays by the rules, these additional regulations just add additional cost and compliance burden, which gets in the way of good care. There is only one class of doctors who afford the time and resources to hiring extra staff to handle specious treatments, and those are the serial abusers of the system. The New Yorker itself did a fine expose piece in 2009 about these serial abusers in McAllen, Texas, who took advantage of low income, non-English speakers to run up costs. This type of abuse would not be possible except that there are large central systems to manipulate, and because they were such abusers, it was worthwhile to devote resources to this manipulation.
We at Lake Washington Sports & Spine will continue to fight against this trend. We will aim to be judicious in use of resources, but we will always prioritize the needs of the patient first.
Thursday, April 23, 2015
Tennis elbow: Not just for tennis players!
Tennis elbow is a significant problem that can prevent people from performing athletically and occupationally. Tennis elbow, or lateral epicondylopathy, is an overuse injury that presents as pain and tenderness on the outside of the elbow. While 50 % of tennis players will develop tennis elbow during their lifetime, they represent only 5% of patients diagnosed with tennis elbow. Plumbers, cooks, auto mechanics and other workers with occupations requiring repetitive gripping and grasping activities represent a large portion of people with LE. People of all ages with overuse can acquire tennis elbow, but most cases of the injury occur in people between the ages of 30 and 50.
So, how do we treat tennis elbow? Lateral epicondylopathy should first be treated with rest, ice and activity modification. For more serious cases, prolotherapy and PRP are great options to amplify the body’s healing response. It’s important to note that cortisone or “steroid” injections should not be used as a temporary quick-fix. Patients often report feeling better at the time of the injection, but often end up with poor future outcomes likely related to a combination of tissue degradation from the cortisone and lack of biomechanical alterations (causing them to re-injure themselves).
A great tool to help see the lateral epicondyle is the use of musculoskeletal ultrasound. Ultrasound is the imaging test of choice for the lateral epicondyle, for a reasons:
1. The highest level of resolution and detail
2. The level of detail is particularly excellent for tendon, ligament, and fascia, which are types of tissue that are not always seen clearly on other imaging tests (e.g., x-rays and MRIs)
3. It is the best test for checking motion
4. It is the only imaging test where we can also test for tenderness (since the ultrasound probe is touching the affected area)
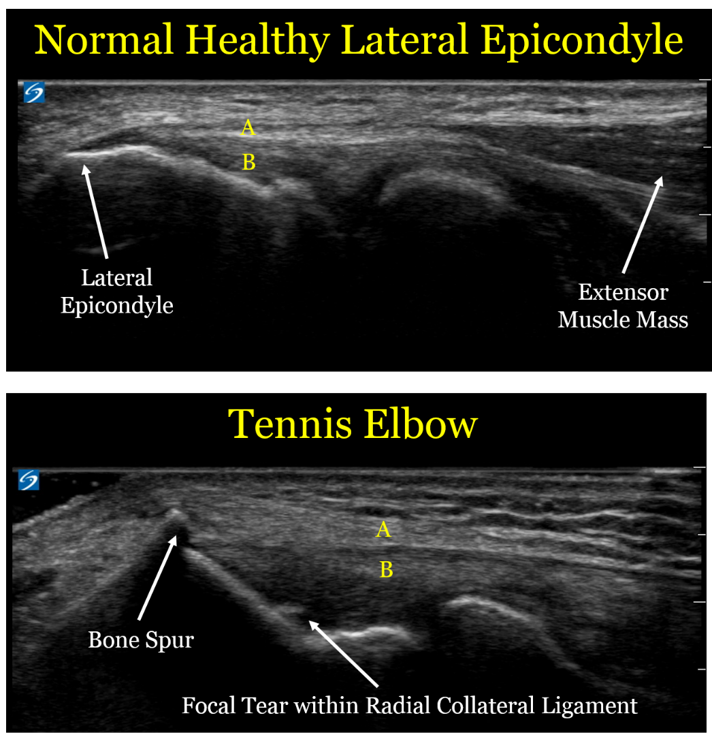
Here are comparison ultrasound images of a healthy lateral epicondyle, followed by the lateral epicondyle of a patient with tennis elbow.
Let's look at the ultrasound images above, first focusing on the upper image of a healthy tendon. One useful thing to see visually is that the muscle mass (the right arrow) looks distinctly different than the extensor tendon (designated by the yellow letter "A"). This is an important detail, since muscle has an excellent blood supply and heals well. Tendon is made of a tight bundle of collagen with a relatively poor blood supply, and may struggle to heal.
In the second image, we can see the anatomic changes associated with tennis elbow:
1. The extensor tendon (A) is thickened and not as well defined as in the healthy elbow. Of note, the patient with the healthy tendon is actually a much larger and more muscular person, so the thickened tendon is in fact a sign of an unhealthy tendon
1. The extensor tendon (A) is thickened and not as well defined as in the healthy elbow. Of note, the patient with the healthy tendon is actually a much larger and more muscular person, so the thickened tendon is in fact a sign of an unhealthy tendon
2. The bone spur created by the unhealthy tendon. We call this an enthesophyte, which is where hte tendon inserts onto the bone. The reason these enthesophytes form is because bone is really a very dense putty, so the enthesophyte is caused by abnormal pulling forces by the unhealthy tendon
3. The part labeled "B" is the radial collateral ligament (RCL), which is underneath the extensor tendon. In the case of the unhealthy patient, there is a tear in the RCL. By definition, a sprain is a tear in a ligament.
4. Of note, there is no "inflammation", which is why the term -itis (e.g., tendonitis) is usually a misnomer. This is an example of a chronic degradation of the extensor tendons and underlying radial collateral ligament, and the more proper term would be tendinosis or tendinopathy.
4. Of note, there is no "inflammation", which is why the term -itis (e.g., tendonitis) is usually a misnomer. This is an example of a chronic degradation of the extensor tendons and underlying radial collateral ligament, and the more proper term would be tendinosis or tendinopathy.
For a sake of comparison, the image below is an MRI
The level of detail is far less. The resolution (which is defined as the ability to distinguish 2 points as distinct) is 5 times higher for the ultrasound. In the ultrasound image, there is a clear distinction between the extensor tendons and the underlying radial collateral ligament, and we can see the individual fibers with great detail. In the MRI, the white arrows show what is essentially a black line, with far less detail. MRI does have some advantages in other contexts (e.g., it sees a wider field of view and can penetrate the bone, so it helps with bone contusions and certain types of joint injuries), but for imaging the lateral epicondyle, ultrasound is a better choice.
So what should we do with these patients?
- Historically, physicians have often performed landmark-based injections to the lateral epicondyle of cortisone. However, moreso than for any other sports injury, repeated data show this is not a good idea. While cortisone injections may help in the short term, they clearly make the injuries worse in the long term.
- Similarly, patients are often advised to use the non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen. However, these are also bad choices, because while they can help with pain in the short term, they also prevent healthy collagen formation.
- The best initial treatment option is repeated icing. Ice is a better anti-inflammatory than any medication, and also has other healing benefits.
- Physical therapy is also a mainstay of the best treatment for tennis elbow, where they can focus on exercise protocols designed to promote healing and fix damaging biomechanical patterns.
- For the subset of patients who do not improve with either ice or physical therapy, we often recommend use of proliferative therapy techniques including platelet-rich plasma injections or prolotherapy, which can help induce healthy healing.
Meet the Team: James Kim!
What is your role on the Team at Lake Washington Sports & Spine?
I
am Dr. Chimes's new medical assistant. I will help patients on their
path to recovery and will do whatever I can to Keep People Active!
As the newest member of our team, we’d love for our patients to get to know you better. Can you tell us 5 facts about James?
1)
I was a Peace Corps volunteer in the country of Armenia from 2011-2013.
Ask me anything about the country itself, what the Peace Corps was
like, or how to live without indoor plumbing!
2)
I'm a new transplant to Seattle! I have previously lived in New York,
Illinois, and New Orleans. I miss Zabar's, Portillo's, and weekly
parades/festivals.
3) I used to work in bicycle shops as a mechanic. Got bike issues? Let me know.
4) The first time I ate raw cookie dough was in 2012.
5) I cannot, for the life of me, figure out how to hula hoop.
When did you first become interested in medicine (or why is the field of sports medicine appealing to you)?
As
a child, I was encouraged (read: pushed) into studying for a career in
either law or medicine. I was naturally inclined towards math and
science, and liked figuring out how things work and how to fix them, so
medicine seemed the right choice. Besides, I was never very good at
arguing. Sports medicine appeals to me because I've always watched
sports, as I grew up in Illinois during peak sports years, i.e. the
Michael Jordan years. I'm also quite active myself, and am continually
fascinated and amazed at the capability of the human body.
What's your favorite form of exercise?
Nothing is more mind-clearing than shooting jumpers in an empty gym.
Do you have a favorite professional athlete? What qualities and characteristics does he possess that make him your favorite?
I
don't have a single favorite, as there are too many great athletes with
characteristics I really admire! But if I had to choose one sport and
one position, I'd say Steve Nash for point guard. He was never the
biggest, fastest, or quickest, but he put up historical numbers by
working harder than most everyone else. He knew his advantages and
refined them, constantly improved his problem areas, and at least once a
game made you wonder "How did he do that?!"
You
are planning a career as a physical therapist. What skills do you hope
to learn here at LWSS before going to graduate school?
I
hope to increase my base of knowledge in anatomy and physiology; learn
more about diagnostic tests and techniques; and how to be a great
medical professional overall.
Thursday, April 16, 2015
7 Reasons why YOU should take a walk TODAY!
1. It's FREE! No expensive exercise equipment or gym membership needed! Just a pair of sneakers, maybe some catchy tunes or a podcast, and a positive attitude!
2. It can help you reach your weight loss goals. Walking quickly for just 30 minutes a day is a great addition to any weight loss regimen! Walking has also been shown to help keep food cravings in check and since we all know that the main factor leading to weight loss is proper nutrition, this is a double bonus!
3. It strengthens and protects your heart. More specifically, it lowers bad (LDL) cholesterol, increases good (HDL) cholesterol and stabilizes blood pressure. That's why you should LOVE walking!
4. It can help prevent osteoporosis & osteoarthritis. Walking is a weight-bearing exercise and helps to strengthen bones, prevent bone thinning and maintain healthy cartilage.
5. It can help improve your sleep. Most of us are not getting nearly enough Z's each night but studies have shown that getting outside for a walk can help regulate our body's melatonin levels, which helps regulate the sleep cycle.
6. It gives you a chance to form relationships. Walking alone with some music or a podcast is fantastic, but so is taking the time to walk with your spouse, your children, or a friend! Plus, buddying up during exercise makes it more enjoyable and, in turn, makes you more likely to stick to the routine. So grab a pal and get walking!
7. It lowers stress and increases happiness! Exercise of any sort releases our body's "happy drugs": endorphins! Endorphins cause that sense of euphoria that comes after physical activity. In addition, they can inhibit the transmission of pain signals. Walking generates endorphins which increase happiness and decrease pain. In other words, walking is medication (insert gasp here)!
Whatever YOUR reason, just strap on a pair of shoes and get walking! The Lake Washington Sports & Spine team will be rooting for you!
2. It can help you reach your weight loss goals. Walking quickly for just 30 minutes a day is a great addition to any weight loss regimen! Walking has also been shown to help keep food cravings in check and since we all know that the main factor leading to weight loss is proper nutrition, this is a double bonus!
3. It strengthens and protects your heart. More specifically, it lowers bad (LDL) cholesterol, increases good (HDL) cholesterol and stabilizes blood pressure. That's why you should LOVE walking!
4. It can help prevent osteoporosis & osteoarthritis. Walking is a weight-bearing exercise and helps to strengthen bones, prevent bone thinning and maintain healthy cartilage.
5. It can help improve your sleep. Most of us are not getting nearly enough Z's each night but studies have shown that getting outside for a walk can help regulate our body's melatonin levels, which helps regulate the sleep cycle.
6. It gives you a chance to form relationships. Walking alone with some music or a podcast is fantastic, but so is taking the time to walk with your spouse, your children, or a friend! Plus, buddying up during exercise makes it more enjoyable and, in turn, makes you more likely to stick to the routine. So grab a pal and get walking!
7. It lowers stress and increases happiness! Exercise of any sort releases our body's "happy drugs": endorphins! Endorphins cause that sense of euphoria that comes after physical activity. In addition, they can inhibit the transmission of pain signals. Walking generates endorphins which increase happiness and decrease pain. In other words, walking is medication (insert gasp here)!
Whatever YOUR reason, just strap on a pair of shoes and get walking! The Lake Washington Sports & Spine team will be rooting for you!
Friday, April 10, 2015
Pursuit of Pure Medicine
Here is a feature on MedPage today about practice's decision to stop taking Medicare. Based on early comments, more and more clinicians are feeling similarly.
Join the crusade to practice Pure Medicine, and put the needs of patients first, rather than the needs of compliance officers!
Join the crusade to practice Pure Medicine, and put the needs of patients first, rather than the needs of compliance officers!
Thursday, April 9, 2015
Great resource on hip mobility and strength
One of out favorite physical therapists, Adam Shildmyer, recently shared a great link on tactics for improving motion during athletic performance, motion, and stability.
Ultrasound Case of the Day- Ganglion Cyst
Today's case focuses on a ganglion cyst of the wrist.
This is the class bump to the back of the wrist that can form as a "wear and tear" injury. In the olden days, these were typically treated by smacking the cyst with a Bible. Bible smacking still works (sometimes), but we can also use ultrasound to help treat the cyst in a less brutal manner
I chose to show this image both because:1. It can help show patients the techniques Dr. Hyman and I use for treating different conditions in a more accurate and less painful way
This is the class bump to the back of the wrist that can form as a "wear and tear" injury. In the olden days, these were typically treated by smacking the cyst with a Bible. Bible smacking still works (sometimes), but we can also use ultrasound to help treat the cyst in a less brutal manner
2. It highlights an advanced technical point for other clinicians learning to use ultrasound
The ganglion cyst is the large black area highlight by the yellow area. It appears large and black because the sound waves from the ultrasound machine penetrate easily through water, so it does not reflect back signal (as does the underlying bone)
The blue and red arrows are pointing to the extensor tendon of the ring finger. This is the tendon that would help straighten out the ring finger if the finger was bent. You can see a series of white parallel fibers that are extending from left to right across the screen. One of the great strengths of ultrasound is that it is a MUCH higher resolution than an MRI. On an MRI, then tendon would like like a simple black line, but using the ultrasound we can see the individual collagen fibers at a much higher level of detail.
The green arrow points at the underlying joints in the wrist (called a carpal joint). This is an advantage of looking at the cyst under ultrasound - in this particular case, we can see that the cyst is very clearly NOT in continuity with the joint. This has significance in terms of risk of infection or other complications
For this specific patient, we drained the cyst using ultrasound guidance. In the past, we used to perform this procedure the way most doctors still do, which is feel around and just stick a needle into it. The reason we use ultrasound guidance is to make sure we are not inadvertently injuring other structures (e.g., the carpal joint or the extensor tendon). I can also do a detailed refinement called a fenestration, where I create multiple small holes in the cyst, which helps prevent the cyst from reforming.
Finally, a technical point for aspiring ultrasonographers- you may notice that the tendon immediately below cyst (the red arrow) is brighter than the tendon that is not beneath the cyst (the blue arrows). This is an artifact called "through transmission." What happens here is that the computer processor used by the ultrasound machine works under the assumption that the tissue density is uniform throughout the width of the ultrasound beam. However, because the sound waves passing through the cyst have very little resistance, the computer processor will make everything deep to the cyst appear more bright (called hyperechoic) than it actually is.
One of the quirks with ultrasound is that because it shows so much detail, it is prone to artifacts that, in the wrong hands, can be misread as pathology in the patient. This is why Dr. Hyman spend so much time travelling across the country working with other physicians to learn more about the nuances of ultrasound
One of the quirks with ultrasound is that because it shows so much detail, it is prone to artifacts that, in the wrong hands, can be misread as pathology in the patient. This is why Dr. Hyman spend so much time travelling across the country working with other physicians to learn more about the nuances of ultrasound
Monday, March 30, 2015
Congratulations, Tony!
As part of our business culture, Lake Washington Sports & Spine
supports & encourages our staff members to chase their dreams and
become the best versions of themselves. We're proud to announce that
Tony, medical assistant extraordinaire, was accepted into the DPT program at UNLV!! We'll
be sad to see him leave the LWSS team, but we are so happy he is on the path
to achieving his career goals! Go Tonyyyyy!!
Wednesday, March 18, 2015
Nutrition: 9 easy ways to get your fruits and vegetables
March is (drum roll...)
NATIONAL NUTRITION MONTH!
We asked our go-to nutritionist, Chelsey Ocean, to offer some simple tweaks to help add more fruits and vegetables to our diets. For more information about Chelsey & the services she offers, visit her at www.myfoodexpert.com
9 easy ways to get your fruits
and vegetables
 |
| Chelsey Ocean, MS, RDN, CD, CSSD |
We all know that fruits and vegetables are
healthy for us and you may even know 5-7 servings of fruit is what you should
aim for on a daily basis. But how can you pack all those healthy servings in
one day? See below for some easy tips to get those fruits and vegetables in
your diet.
Breakfast
- Add spinach, kale and/or celery to a fruit based smoothie. It may turn the smoothie green, but with the sweetness of the fruit you will never know where that green color is coming from!
- Make a parfait with 0% plain Greek yogurt, fruit, nuts, cinnamon, mix and serve
- A chicken sausage, egg white scramble with mushrooms, onions, and peppers makes a high veggie protein meal
Lunch
- Use romaine lettuce leaves to make deli meat sandwiches or wrap your turkey burger with in a lettuce blanket
- Take a cantaloupe, cut in half, remove seeds and serve inside a scoop of tuna mixed with salsa
- Add cooked or pureed cauliflower, peas or squash to mac and cheese
Dinner
- Use spaghetti squash instead of noodles and serve with turkey meatball, marinara or parmesan
- Make a salad with at least three colors of the rainbow: red, green and purple (tomato, romaine lettuce, and purple cabbage)
- Make a mixed berry blend of strawberries, raspberries and blueberries sprinkled with vanilla extract, cinnamon, cardamom and clove serve as a sweet after dinne
Monday, March 16, 2015
The Health Cost of Complexity: the concept of Time Debt
This link from the Harvard Business Review does an outstanding job explaining the concept of "Time Debt."
One of the most common problem I run into with patients is that they have too much on their plate, and this leads to health consequences. When the body is in a perpetual time debt state, the sympathetic nervous system kicks in, which is something physicians call "sympathetic overload."
The sympathetic nervous system is designed to handle our "fight or flight" response. This is an appropriate response to being chased by a Tiger, or dealing with the occasional busy work deadline.
However, we as human beings were NOT meant to be in a state of constant "fight or flight," and our body does not handle it well. Persistent sympathetic flow can lead to agitation, weight gain, poorly healing injuries, heart attacks, and death.
There is a great scene in the movie Parenthood, where Steve Martin's character Gil is confronted with a list of things he needs to do. His wife asks him if he has to do something, and Gil responds "my whole LIFE is have to."
That sense of HAVING to do things is what drives the sense of Time Debt stress. What I advocate patients do, to prioritize their health, is to re-evaluate the "Have to" items in their life.
This can often lead to some challenging decisions- you may need to re-evaluate your entire life. When I was in the my late 30s, I realized my life was filled with too many "Have tos" in my life, which led to my decision to leave Academic Medicine, move across the county, and start prioritizing my own health.
Simplifying your life is not easy to do. However, just because it is challenging to embrace simplicity doesn't make the concept less important. It makes embracing simplicity MORE important.
One of the most common problem I run into with patients is that they have too much on their plate, and this leads to health consequences. When the body is in a perpetual time debt state, the sympathetic nervous system kicks in, which is something physicians call "sympathetic overload."
The sympathetic nervous system is designed to handle our "fight or flight" response. This is an appropriate response to being chased by a Tiger, or dealing with the occasional busy work deadline.
However, we as human beings were NOT meant to be in a state of constant "fight or flight," and our body does not handle it well. Persistent sympathetic flow can lead to agitation, weight gain, poorly healing injuries, heart attacks, and death.
There is a great scene in the movie Parenthood, where Steve Martin's character Gil is confronted with a list of things he needs to do. His wife asks him if he has to do something, and Gil responds "my whole LIFE is have to."
That sense of HAVING to do things is what drives the sense of Time Debt stress. What I advocate patients do, to prioritize their health, is to re-evaluate the "Have to" items in their life.
This can often lead to some challenging decisions- you may need to re-evaluate your entire life. When I was in the my late 30s, I realized my life was filled with too many "Have tos" in my life, which led to my decision to leave Academic Medicine, move across the county, and start prioritizing my own health.
Simplifying your life is not easy to do. However, just because it is challenging to embrace simplicity doesn't make the concept less important. It makes embracing simplicity MORE important.
Thursday, March 5, 2015
Accountability: How to Achieve Your Goals
As we are approaching the annual “spring forward” this
Sunday, I have begun reflecting on New Year’s resolutions. Maybe it’s losing the extra weight they put
on over the holiday season, maybe it’s training to run one 5K per month, or
maybe, like me, they are planning on taking a graduate school entrance exam
(MCAT here I come!) When reading through
your resolutions list, many may sound like the ghosts of resolutions past. How many times have each of us said “Now THIS
is the year that I do [enter resolution here]!”? And yet, as late spring rolls around, our
running shoes have collected dust, our pantry is filled with unhealthy snacks
that we are not keeping track of, and our study supplies are packed away in
storage. We start to make excuses – “I’ve
been overwhelmed with a project at work”, “I was busy with my kids”, “I don’t
have the money for a gym membership”, etc.
These excuses allow us to relapse into old habits and forget the resolve
we had in January. I mean, there’s always next year, right??
Now for some of us (myself included) there comes a point when
we desperately want to break away from this cycle and finally achieve these New
Year’s resolutions, becoming the better versions of ourselves. When that time
comes, accountability is a major
asset.
Simply by having another person, whether it’s a couple of people, or
your entire list of Facebook friends list aware of the goals you have set for
yourself makes it a lot harder to skip that morning jog, opting instead for a
muffin at Starbucks.
Personally, I am absolutely guilty of “recycling” my
resolutions. I have found that
accountability has become my ultimate sidekick, the most powerful tool that
keeps me going. Take the MCAT (the
medical school entrance exam), for
example. I have told anybody who will
listen that I plan to take the infamous exam at the beginning of this
summer. I have explicitly set up a study
schedule and I text my mom every night after I’m done with my session. If I don’t text her, she usually texts me
(she’s very on top of her game. Go Mom!) Although I don’t want to disappoint myself by
doing poorly on the exam, I certainly
don’t want to disappoint her (or any other friends who have been patient and
unwavering in their support through this journey).
This same idea can be applied to the different treatment
options that Drs. Hyman and Chimes recommend to their patients. If 30 minutes of daily exercise is what the
doctor ordered and you know that there might be days when the devil on your
shoulder tells you to skip the gym and stay in bed, enlist a friend to come
along! First of all, you’re much less likely to flake out on a friend than you
are on yourself. Second, the exercise
will be much more fun with a friendly face right there, pounding the pavement
with you, in turn, making it more likely that you’ll form a healthy new habit! If one of the treatment recommendations is
tracking your food intake, whether on paper or in a food tracking app like www.myfitnesspal.com, send a copy of
each day’s intake to somebody, such as your spouse, your nutritionist, or
personal trainer.
Another way to be held accountable is to have money on the
line. Spending $300 to take the MCAT
definitely makes me only want to take it once,
and that motivates me to stick to a strict study schedule. In regards to
exercise, one can sign up for a paid class or a personal trainer. It is much harder to miss a workout when you
know it will cost you a $70 training session or a $25 exercise class. Knowing that there is money on the line
certainly makes each of us more likely to follow through. You probably would not skip out on your
massage appointment; so don’t skip out on your workout!
Whichever method of accountability you choose, the doctors
and staff at Lake Washington Sports and Spine are here to support you on the
path to achieving those New Year’s resolutions and becoming the best version of
yourself!
Tuesday, March 3, 2015
Ceasing Medicare Contract: Frequently Asked Questions
What
Underpins Our Decision?
Our decision to stop contracting with
CMS is based upon the simple premise that we wish to provide the best,
unfettered, unobstructed care. Care influenced only by what will best
serve the patient. We feel that CMS (and to a lesser extent, other insurers)
continue to evolve and create policy with the goal being cost control, at times
under the guise of improving quality.
A very significant, though secondary
reason, for discontinuing our contract with CMS is that the finances do not
make sense. Cuts in payments in many cases mean that our business
liabilities exceed our reimbursements. Our business certainly cannot
sustain this trend of increasing costs and diminishing returns. We aim to
take control of and stabilize our financial circumstances, so we may continue
to serve the sports medicine needs of the Eastside and greater Seattle
community for many years to come.
What
Does the Evidence Say?
It is a misnomer that scientific data,
or "Evidence-Based Medicine" (EBM), is always available to guide us,
the medical providers. Even in the best of circumstances, when
well-designed research studies are available to guide us, this is
"evidence-informed medicine" -- meaning that one has to carefully
interpret the research and apply deliberately as appropriate to the unique
circumstances of an individual patient.
Moreover, CMS has manipulated the interpretation of data, selectively
favoring research that restricts access for patients and conveniently
disregarding research that favors promising techniques. As cutting edge clinicians, this limits our
toolbox for helping patients.
What
Can You Do?
We would advise you to learn more about
the evolving changes in healthcare and the risks posed to you as the healthcare
consumer. Then write your local, state, and federal representatives to
express your opinions. This impacts you, now, and your children and
grandchildren in the future.
We also advise that when it comes to
money and health that you budget for total health cost, which includes health
insurance premiums, ancillary health insurance payments (copays, deductible, co-insurance),
gym membership, and food. Many patients
only consider health insurance premiums and are caught off-guard by these other
predictable expenses.
Can
You Still Receive Medical Care from Us?
Yes. Though you would have to sign
some official paperwork consenting to receive treatment from a non-contracted
Medicare provider, we would be happy to treat you in so long as we are the best
fit to assist you. We accept cash for our professional services.
Our goal is to restore you to optimal function as quickly as possible.
What
if I'm Referred to Another Provider? Can I Use My Insurance?
It depends. If the provider to
whom you are referred is a contracted provider through Medicare/CMS, then you
may use your insurance.
Opting out of Medicare
Following a long period of deliberate
contemplation, we, the physicians of Lake Washington Sports & Spine, have
decided to cancel our contract with the Center for Medicare Services
(CMS). This will take effect as of April 1, 2015.
As board-certified Sports Medicine
providers, with the primary mission of keeping people active (KPA!), we cannot
in good faith continue this relationship as our mission no longer appears to
align with that of CMS.
To clarify, this means that Drs. Hyman
and Chimes will no longer process Medicare insurance claims in our office as of
April 1, 2015.
We'd like to explain our decision, at
least in brief.
The Medicare trust account is
underfunded. This is well established. The fund is expected now to
be depleted by ~2030. Over a period of years, CMS has set in process
several measures to reduce healthcare payments to providers caring for Medicare
beneficiaries, or to eliminate coverage altogether for some effective and
well-established services.
For example, one spinal injection called
a therapeutic cervical facet joint injection is no longer covered, despite its
effectiveness for many patients. Other procedures that show promise such
as prolotherapy and platelet-rich plasma (PRP) injections for refractory
chronic tendon and joint problems are not covered, while CMS continues to cover
steroid ("Cortisone") injections even in light of very limited
evidence to support them. These policies make no sense, not for sports
medicine providers, nor sports medicine patients.
Despite the many additional years of
highly specialized training required to perform nerve testing, spinal
injections and musculoskeletal ultrasound (above and beyond that necessary for
our Board certification), CMS is reducing reimbursements for these services in
dramatic fashion: nerve testing has been cut by >50%, >60% in cuts
for certain cervical spinal injections and 2015 will bring cuts of nearly 75%
on ultrasound guided injections. In the
past, physicians have absorbed the small incremental cuts in payment, but, because
these cuts are so dramatic, the payments now in many cases are insufficient to cover the cost of doing
business.
New similar policies are set in place
each year. These global policies are most certainly designed to limit
access to care, deliberately to reduce costs.
Our primary goal is to provide the
absolute best care for patients who choose to seek our professional advice, and
to restore those patients to optimal function using the best possible tools at our disposal.
And so therein lies the conflict.
We are focused on caring for and improving the health and wellbeing of
our patients and our community. CMS's
goal is to reduce healthcare dollar spending in the United States.
Additionally, Medicare has been hiring
bounty hunters called RAC's to review charts to look for errors in coding (and
medical coding is unnecessarily complex) to charge physicians with fraud, and
fine hundreds of thousands of dollars or in some cases send physicians to
federal prison. So not only is CMS reducing our reimbursement, but it is
placing physicians’ billing practices under a microscope, looking to recoup
millions of dollars and to criminalize and make examples of physicians.
While we are certain that our clinic's practices would hold up to the
greatest scrutiny, we would rather not continue on this booby-trapped playing
field.
We are confident that this decision will
positively influence our patients, and will more than ever, align patient and
physician goals. We recognize that our decision may cause anxiety or
angst for some of you. Should one wish to continue to treat in our clinic
on a 'cash pay' basis, yet have concerns about ability to pay, we ask that they
please contact us to discuss these concerns. We will do everything possible
to ensure patients receive the care they need.
For additional reading, please refer to :
http://lakewass.blogspot.com/2015/03/ceasing-medicare-contract-frequently.html
http://lakewass.blogspot.com/2015/03/ceasing-medicare-contract-frequently.html
Wednesday, January 28, 2015
Sunday, January 25, 2015
An excellent link showing how Medicare bullies and abuses physicians
A colleague of mine forwarded me a great link from the excellent blog KevinMD
In the link, there is a video from a rural physician named Karen Smith, testifying about the harassment she received from Medicare for errors made by the organization administering Medicare, the Center for Medicare and Medicaid Services
An increasing number of physicians, including us, are realizing that the abusive tactics used by Medicare are preventing us from care from senior patients in the way they deserve to be treated.
In the link, there is a video from a rural physician named Karen Smith, testifying about the harassment she received from Medicare for errors made by the organization administering Medicare, the Center for Medicare and Medicaid Services
An increasing number of physicians, including us, are realizing that the abusive tactics used by Medicare are preventing us from care from senior patients in the way they deserve to be treated.
Tuesday, January 20, 2015
Physicians Corner: Advantage of Single Leg Squats & Lunges
*Please pardon our video quality. We specialize in musculoskeletal medicine, not video production.
Subscribe to:
Posts (Atom)










.jpg)