I saw a fascinating case last month. The patient was a high level 13 year old baseball player who developed pain in the region of his knee cap (technically called the patella).
He did not have any traumatic injury, so I had a low suspicion of an injury like a patellar fracture, nor did I suspect a traumatic injury his ACL ligament or meniscus.
He was just starting his growth spurt. Youth athletes are vulnerable to a different class of injuries than adult athletes. The patellar ligament is what I call a structural complex, connecting the lower portion of the knee cap (the inferior pole of the patella) to a small bump on the shin called the tibial tuberosity.
This patellar ligament complex can be injured in different locations, depending on age:
- Age 11-12- at the inferior pole of the patella, an injury called Sinding-Larsen-Johannson syndrome
- Age 13-14- at the tibial tuberosity (where the patellar ligament attaches to the tibia)- called Osgood Schlatter syndrome.
The age ranges for SLJ and OS are approximate, but as a general rule SLJ occurs earlier in adolescence, and the more common OS occurs a few years later. Their timing is based on when the bony processes, called an apophysis, fuses to the rest of the bone.
By late adolescence, the apophyses have fully fused, so we don't see these injuries much by an athlete's late 20s. We may still see irregularities in the bone, but these are remnants of a prior injury, and rarely the cause of injury itself. Instead, in athletes who are past puberty, the most common site of injury is within the patellar ligament itself (usually closer to the patella than the tibial tuberosity), a a condition called patellar tendinopathy, or jumper's knee.
In our clinic at Lake Washington Sports & Spine, Dr. Hyman and I like to use high-resolution musculoskeletal ultrasound to image the patellar ligament complex. Ultrasound is a particularly great imaging tool for assessing tendons, for the following reasons:
1. It has the highest spatial resolution- 5-10 times higher than MRI
2. Real time assessment- it is the only imaging test that adds in actually touching the patient, so we can confirm that the area being imaged is actually painful. This is particularly valuable in rough-and-tumble athletes with a history of prior injuries, to help clarify whether the injury is new
3. Fantastic tissue differential- ultrasound is great at distinguishing between different tissue types
To give an example of an ultrasound image of a patellar-ligament complex injury, the image below is that of Sinding Larsen Johannson syndrome in an 11 year-old elite-level soccer player. The yellow box shows irregularity in the apophysis of the inferior pole of the patella (to help with orientation, left is superior, right is inferior)
Getting back to the 13 year old baseball player, based on his age and pain near the patella, I was anticipating that he may have SLJ syndrome. However, his pain was located higher (on the superolateral portion of his knee cap).
Indeed, as the image below shows, the patella looked pristine in the center, with a smooth cortex
However, when I moved the probe laterally, I could see two disruptions in his cortex
This is a case of what is called a bipartite patella. The superolateral portion of the patella never fused to the remaining part of the patella. The x-ray image below shows the non-union of the bipartite patella, along with the planes of the two images above
How did I use this information clinically:
1. Relative non-use
2. Physical therapy. Particular focus include stretching of the rectus femoris at the hip, since we wanted to limit traction of the quad distally
3. Avoiding NSAIDs. The specific mechanism can interfere with healthy collagen synthesis, essential in this growing athlete
4. Regular icing
This athlete did great, and was able to return to sport in 1 month
Tuesday, May 26, 2015
Wednesday, May 6, 2015
Exercise Is Medicine! Dr. Hyman Trains with the US Medical Soccer Team in Atlanta (www.usmedicalsoccerteam.org)
May 2015
I just returned from a wonderful weekend devoted to community service, physician-kinship and arduous physical training in Atlanta, Georgia.
I met up with approximately 30 other physician colleagues from around the USA to prepare for our upcoming hosting of the World Medical Football Congress (WMFC), set to take place in Long Beach, CA, at the end of June 2015. We are the US physicians who make up the US Medical Soccer Team (USMST). (www.usmedicalsoccerteam.org)
We had 4 separate training sessions over the weekend and now I am enjoying a day of muscle recovery (but brain exercise) at work. Our coach performed well to get us organized into a formation that should allow us to win games and make it to the knock out round of the tournament.
We arrived Friday afternoon, and met at the GW Carver Boys & Girls Club of Metro Atlanta, and we delivered our own “Healthy, Fit and Smart” education program to approximately 100 disadvantaged children. The kids were wonderful — engaging, energetic, and with every small success answering our questions, their eyes beamed, and the potential for these children to absorb knowledge like sponges was palpable. Highlights included one child answering ‘potassium’ as one of the 5 food groups (e.g. fruits, vegetables, grains, meats/fish, dairy), and another answering “eight hours a day” for the minimum time doctors recommend children watch TV (to be clear, there are no minimum daily requirements for TV watching!). I think all of us doctors left the event grateful to the children from whom we continue to learn each time we deliver the Healthy, Fit and Smart program.
Our USMST potential is strong. We will compete against physician national soccer teams from 18 different countries. We’ve not made it past the early stages in prior tournaments. In truth, we are a perennial underdog. This year the team has several new physician-athletes, and we have high hopes to make our way to the knock out round of the tournament.
The physicians with whom I play are from all fields, and many are naturalized US citizens. We have a trauma surgeon originally from Caracas, Venezuela, a vascular surgeon from Lima, Peru, an Internist from Romania, and a Family Physician from Trinidad and Tobago. A good number of our physicians are originally from Iran. We are a real melting pot. Our dinner conversation usually surrounds soccer, but of course we banter quite a bit about medical topics as well.
So as our June training in Seattle and our summer tournament draw near, I reflect on how grateful I am that I can continue to push my fitness to new levels and compete on a ‘mini-world stage.’ I thank my family and my work team at LWSS without who's support I could not make this happen.
Monday, May 4, 2015
The danger of the "cost containment" industry
There is a recent article in the New Yorker that highlights the dangers of health care over-utilization. It is a thoughtful, well-written article.
However, I suspect the governmental reaction to this article will be very anti-patient. As an example, one of the major insurance companies we work with just published a bulletin requiring many musculoskeletal injections to undergo prior authorization by an outside company, CareCore National. Their "Musculoskeletal Pain Management Criteria" document is 134 pages of guidelines that will limit what physicians are able to perform in office.
The current "big medicine" solution to over-utilization is to create an extra-layer in the health care process, and that extra layer has a large cost. As a consequence, of the total money the US spends on health care, a higher % will go to administration, and a lower % will go to the actual delivery of care.
One of the terms that is thrown around a lot in medicine is "third party." What patients need to recognize is that when there are increasing bureaucratic layers added in healthcare, the PATIENT becomes the third party. We have many patients who have left big-system medicine practices and are now seen by us, because they are sick of being treated like a widget. This happens because the physician is so busy focusing on compliance requirements from the insurance company and/or the health system where the physician is employed.
Are there people who abuse the system? Of course! But government intervention actually leads to MORE abuse. For the small clinical practice who plays by the rules, these additional regulations just add additional cost and compliance burden, which gets in the way of good care. There is only one class of doctors who afford the time and resources to hiring extra staff to handle specious treatments, and those are the serial abusers of the system. The New Yorker itself did a fine expose piece in 2009 about these serial abusers in McAllen, Texas, who took advantage of low income, non-English speakers to run up costs. This type of abuse would not be possible except that there are large central systems to manipulate, and because they were such abusers, it was worthwhile to devote resources to this manipulation.
We at Lake Washington Sports & Spine will continue to fight against this trend. We will aim to be judicious in use of resources, but we will always prioritize the needs of the patient first.
However, I suspect the governmental reaction to this article will be very anti-patient. As an example, one of the major insurance companies we work with just published a bulletin requiring many musculoskeletal injections to undergo prior authorization by an outside company, CareCore National. Their "Musculoskeletal Pain Management Criteria" document is 134 pages of guidelines that will limit what physicians are able to perform in office.
The current "big medicine" solution to over-utilization is to create an extra-layer in the health care process, and that extra layer has a large cost. As a consequence, of the total money the US spends on health care, a higher % will go to administration, and a lower % will go to the actual delivery of care.
One of the terms that is thrown around a lot in medicine is "third party." What patients need to recognize is that when there are increasing bureaucratic layers added in healthcare, the PATIENT becomes the third party. We have many patients who have left big-system medicine practices and are now seen by us, because they are sick of being treated like a widget. This happens because the physician is so busy focusing on compliance requirements from the insurance company and/or the health system where the physician is employed.
Are there people who abuse the system? Of course! But government intervention actually leads to MORE abuse. For the small clinical practice who plays by the rules, these additional regulations just add additional cost and compliance burden, which gets in the way of good care. There is only one class of doctors who afford the time and resources to hiring extra staff to handle specious treatments, and those are the serial abusers of the system. The New Yorker itself did a fine expose piece in 2009 about these serial abusers in McAllen, Texas, who took advantage of low income, non-English speakers to run up costs. This type of abuse would not be possible except that there are large central systems to manipulate, and because they were such abusers, it was worthwhile to devote resources to this manipulation.
We at Lake Washington Sports & Spine will continue to fight against this trend. We will aim to be judicious in use of resources, but we will always prioritize the needs of the patient first.
Thursday, April 23, 2015
Tennis elbow: Not just for tennis players!
Tennis elbow is a significant problem that can prevent people from performing athletically and occupationally. Tennis elbow, or lateral epicondylopathy, is an overuse injury that presents as pain and tenderness on the outside of the elbow. While 50 % of tennis players will develop tennis elbow during their lifetime, they represent only 5% of patients diagnosed with tennis elbow. Plumbers, cooks, auto mechanics and other workers with occupations requiring repetitive gripping and grasping activities represent a large portion of people with LE. People of all ages with overuse can acquire tennis elbow, but most cases of the injury occur in people between the ages of 30 and 50.
So, how do we treat tennis elbow? Lateral epicondylopathy should first be treated with rest, ice and activity modification. For more serious cases, prolotherapy and PRP are great options to amplify the body’s healing response. It’s important to note that cortisone or “steroid” injections should not be used as a temporary quick-fix. Patients often report feeling better at the time of the injection, but often end up with poor future outcomes likely related to a combination of tissue degradation from the cortisone and lack of biomechanical alterations (causing them to re-injure themselves).
A great tool to help see the lateral epicondyle is the use of musculoskeletal ultrasound. Ultrasound is the imaging test of choice for the lateral epicondyle, for a reasons:
1. The highest level of resolution and detail
2. The level of detail is particularly excellent for tendon, ligament, and fascia, which are types of tissue that are not always seen clearly on other imaging tests (e.g., x-rays and MRIs)
3. It is the best test for checking motion
4. It is the only imaging test where we can also test for tenderness (since the ultrasound probe is touching the affected area)
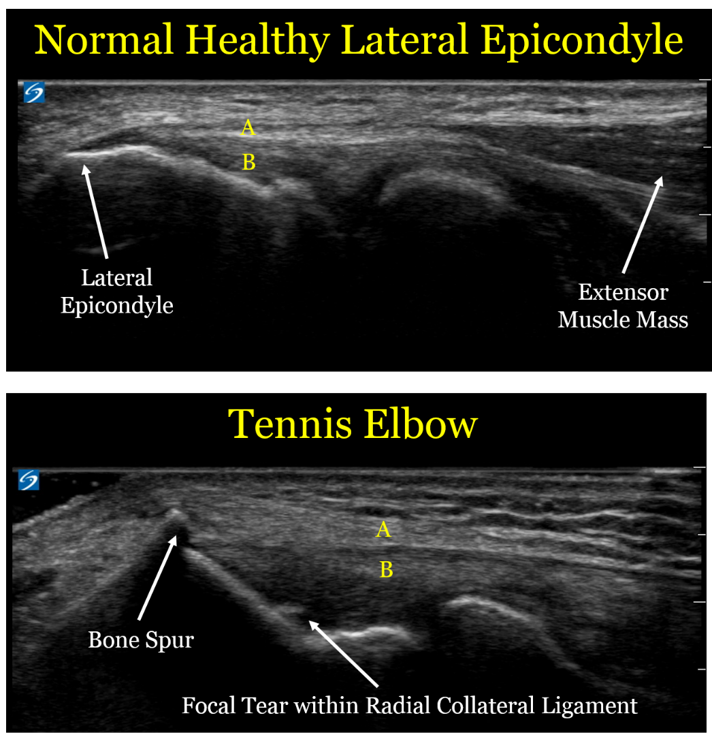
Here are comparison ultrasound images of a healthy lateral epicondyle, followed by the lateral epicondyle of a patient with tennis elbow.
Let's look at the ultrasound images above, first focusing on the upper image of a healthy tendon. One useful thing to see visually is that the muscle mass (the right arrow) looks distinctly different than the extensor tendon (designated by the yellow letter "A"). This is an important detail, since muscle has an excellent blood supply and heals well. Tendon is made of a tight bundle of collagen with a relatively poor blood supply, and may struggle to heal.
In the second image, we can see the anatomic changes associated with tennis elbow:
1. The extensor tendon (A) is thickened and not as well defined as in the healthy elbow. Of note, the patient with the healthy tendon is actually a much larger and more muscular person, so the thickened tendon is in fact a sign of an unhealthy tendon
1. The extensor tendon (A) is thickened and not as well defined as in the healthy elbow. Of note, the patient with the healthy tendon is actually a much larger and more muscular person, so the thickened tendon is in fact a sign of an unhealthy tendon
2. The bone spur created by the unhealthy tendon. We call this an enthesophyte, which is where hte tendon inserts onto the bone. The reason these enthesophytes form is because bone is really a very dense putty, so the enthesophyte is caused by abnormal pulling forces by the unhealthy tendon
3. The part labeled "B" is the radial collateral ligament (RCL), which is underneath the extensor tendon. In the case of the unhealthy patient, there is a tear in the RCL. By definition, a sprain is a tear in a ligament.
4. Of note, there is no "inflammation", which is why the term -itis (e.g., tendonitis) is usually a misnomer. This is an example of a chronic degradation of the extensor tendons and underlying radial collateral ligament, and the more proper term would be tendinosis or tendinopathy.
4. Of note, there is no "inflammation", which is why the term -itis (e.g., tendonitis) is usually a misnomer. This is an example of a chronic degradation of the extensor tendons and underlying radial collateral ligament, and the more proper term would be tendinosis or tendinopathy.
For a sake of comparison, the image below is an MRI
The level of detail is far less. The resolution (which is defined as the ability to distinguish 2 points as distinct) is 5 times higher for the ultrasound. In the ultrasound image, there is a clear distinction between the extensor tendons and the underlying radial collateral ligament, and we can see the individual fibers with great detail. In the MRI, the white arrows show what is essentially a black line, with far less detail. MRI does have some advantages in other contexts (e.g., it sees a wider field of view and can penetrate the bone, so it helps with bone contusions and certain types of joint injuries), but for imaging the lateral epicondyle, ultrasound is a better choice.
So what should we do with these patients?
- Historically, physicians have often performed landmark-based injections to the lateral epicondyle of cortisone. However, moreso than for any other sports injury, repeated data show this is not a good idea. While cortisone injections may help in the short term, they clearly make the injuries worse in the long term.
- Similarly, patients are often advised to use the non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen. However, these are also bad choices, because while they can help with pain in the short term, they also prevent healthy collagen formation.
- The best initial treatment option is repeated icing. Ice is a better anti-inflammatory than any medication, and also has other healing benefits.
- Physical therapy is also a mainstay of the best treatment for tennis elbow, where they can focus on exercise protocols designed to promote healing and fix damaging biomechanical patterns.
- For the subset of patients who do not improve with either ice or physical therapy, we often recommend use of proliferative therapy techniques including platelet-rich plasma injections or prolotherapy, which can help induce healthy healing.
Meet the Team: James Kim!
What is your role on the Team at Lake Washington Sports & Spine?
I
am Dr. Chimes's new medical assistant. I will help patients on their
path to recovery and will do whatever I can to Keep People Active!
As the newest member of our team, we’d love for our patients to get to know you better. Can you tell us 5 facts about James?
1)
I was a Peace Corps volunteer in the country of Armenia from 2011-2013.
Ask me anything about the country itself, what the Peace Corps was
like, or how to live without indoor plumbing!
2)
I'm a new transplant to Seattle! I have previously lived in New York,
Illinois, and New Orleans. I miss Zabar's, Portillo's, and weekly
parades/festivals.
3) I used to work in bicycle shops as a mechanic. Got bike issues? Let me know.
4) The first time I ate raw cookie dough was in 2012.
5) I cannot, for the life of me, figure out how to hula hoop.
When did you first become interested in medicine (or why is the field of sports medicine appealing to you)?
As
a child, I was encouraged (read: pushed) into studying for a career in
either law or medicine. I was naturally inclined towards math and
science, and liked figuring out how things work and how to fix them, so
medicine seemed the right choice. Besides, I was never very good at
arguing. Sports medicine appeals to me because I've always watched
sports, as I grew up in Illinois during peak sports years, i.e. the
Michael Jordan years. I'm also quite active myself, and am continually
fascinated and amazed at the capability of the human body.
What's your favorite form of exercise?
Nothing is more mind-clearing than shooting jumpers in an empty gym.
Do you have a favorite professional athlete? What qualities and characteristics does he possess that make him your favorite?
I
don't have a single favorite, as there are too many great athletes with
characteristics I really admire! But if I had to choose one sport and
one position, I'd say Steve Nash for point guard. He was never the
biggest, fastest, or quickest, but he put up historical numbers by
working harder than most everyone else. He knew his advantages and
refined them, constantly improved his problem areas, and at least once a
game made you wonder "How did he do that?!"
You
are planning a career as a physical therapist. What skills do you hope
to learn here at LWSS before going to graduate school?
I
hope to increase my base of knowledge in anatomy and physiology; learn
more about diagnostic tests and techniques; and how to be a great
medical professional overall.
Thursday, April 16, 2015
7 Reasons why YOU should take a walk TODAY!
1. It's FREE! No expensive exercise equipment or gym membership needed! Just a pair of sneakers, maybe some catchy tunes or a podcast, and a positive attitude!
2. It can help you reach your weight loss goals. Walking quickly for just 30 minutes a day is a great addition to any weight loss regimen! Walking has also been shown to help keep food cravings in check and since we all know that the main factor leading to weight loss is proper nutrition, this is a double bonus!
3. It strengthens and protects your heart. More specifically, it lowers bad (LDL) cholesterol, increases good (HDL) cholesterol and stabilizes blood pressure. That's why you should LOVE walking!
4. It can help prevent osteoporosis & osteoarthritis. Walking is a weight-bearing exercise and helps to strengthen bones, prevent bone thinning and maintain healthy cartilage.
5. It can help improve your sleep. Most of us are not getting nearly enough Z's each night but studies have shown that getting outside for a walk can help regulate our body's melatonin levels, which helps regulate the sleep cycle.
6. It gives you a chance to form relationships. Walking alone with some music or a podcast is fantastic, but so is taking the time to walk with your spouse, your children, or a friend! Plus, buddying up during exercise makes it more enjoyable and, in turn, makes you more likely to stick to the routine. So grab a pal and get walking!
7. It lowers stress and increases happiness! Exercise of any sort releases our body's "happy drugs": endorphins! Endorphins cause that sense of euphoria that comes after physical activity. In addition, they can inhibit the transmission of pain signals. Walking generates endorphins which increase happiness and decrease pain. In other words, walking is medication (insert gasp here)!
Whatever YOUR reason, just strap on a pair of shoes and get walking! The Lake Washington Sports & Spine team will be rooting for you!
2. It can help you reach your weight loss goals. Walking quickly for just 30 minutes a day is a great addition to any weight loss regimen! Walking has also been shown to help keep food cravings in check and since we all know that the main factor leading to weight loss is proper nutrition, this is a double bonus!
3. It strengthens and protects your heart. More specifically, it lowers bad (LDL) cholesterol, increases good (HDL) cholesterol and stabilizes blood pressure. That's why you should LOVE walking!
4. It can help prevent osteoporosis & osteoarthritis. Walking is a weight-bearing exercise and helps to strengthen bones, prevent bone thinning and maintain healthy cartilage.
5. It can help improve your sleep. Most of us are not getting nearly enough Z's each night but studies have shown that getting outside for a walk can help regulate our body's melatonin levels, which helps regulate the sleep cycle.
6. It gives you a chance to form relationships. Walking alone with some music or a podcast is fantastic, but so is taking the time to walk with your spouse, your children, or a friend! Plus, buddying up during exercise makes it more enjoyable and, in turn, makes you more likely to stick to the routine. So grab a pal and get walking!
7. It lowers stress and increases happiness! Exercise of any sort releases our body's "happy drugs": endorphins! Endorphins cause that sense of euphoria that comes after physical activity. In addition, they can inhibit the transmission of pain signals. Walking generates endorphins which increase happiness and decrease pain. In other words, walking is medication (insert gasp here)!
Whatever YOUR reason, just strap on a pair of shoes and get walking! The Lake Washington Sports & Spine team will be rooting for you!
Friday, April 10, 2015
Pursuit of Pure Medicine
Here is a feature on MedPage today about practice's decision to stop taking Medicare. Based on early comments, more and more clinicians are feeling similarly.
Join the crusade to practice Pure Medicine, and put the needs of patients first, rather than the needs of compliance officers!
Join the crusade to practice Pure Medicine, and put the needs of patients first, rather than the needs of compliance officers!
Subscribe to:
Comments (Atom)